Detachment
Vitreous Detachment: What is it?
The posterior chamber of the eye, behind the lens, retains its shape by the presence of vitreous body. This transparent gelatinous "fluid" is uniformly attached to the retina (fig.1 - vitreous humor). As we get older, the vitreous humor gradually shrinks and separates from the retina. In most cases, vitreous detachment is not sight-threatening and requires no special treatment.
When and how does it occur?
As mentioned above, vitreous detachment is an age-relative phenomenon and is more common for older adults (over 60 years old). However, it can also occur in younger people with severe myopia or even after eye injury. Patients describe "floaters", cobweb' or black small 'dots' that suddenly appear and follow eye movements. They may also see "flashes of light" (photopsias), due to vitreous traction.
What should the patient do?
Vitreous detachment does not require special treatment. However, if you see floaters or flashes of light, you should immediately consult an ophthalmologist, who will assess your eye and inform you on what you need to know. The ophthalmologist will also exclude the major complication of vitreous detachment, the retinal tear, which may result in retinal detachment threatening your vision.
Retinal Detachment: What is it?
Under certain circumstances, the retina can peel away from its normal position. For example, if a retinal tear occurs due to vitreous detachment or trauma on its surface, and is not repaired early, the retina may be detached and threaten your vision.
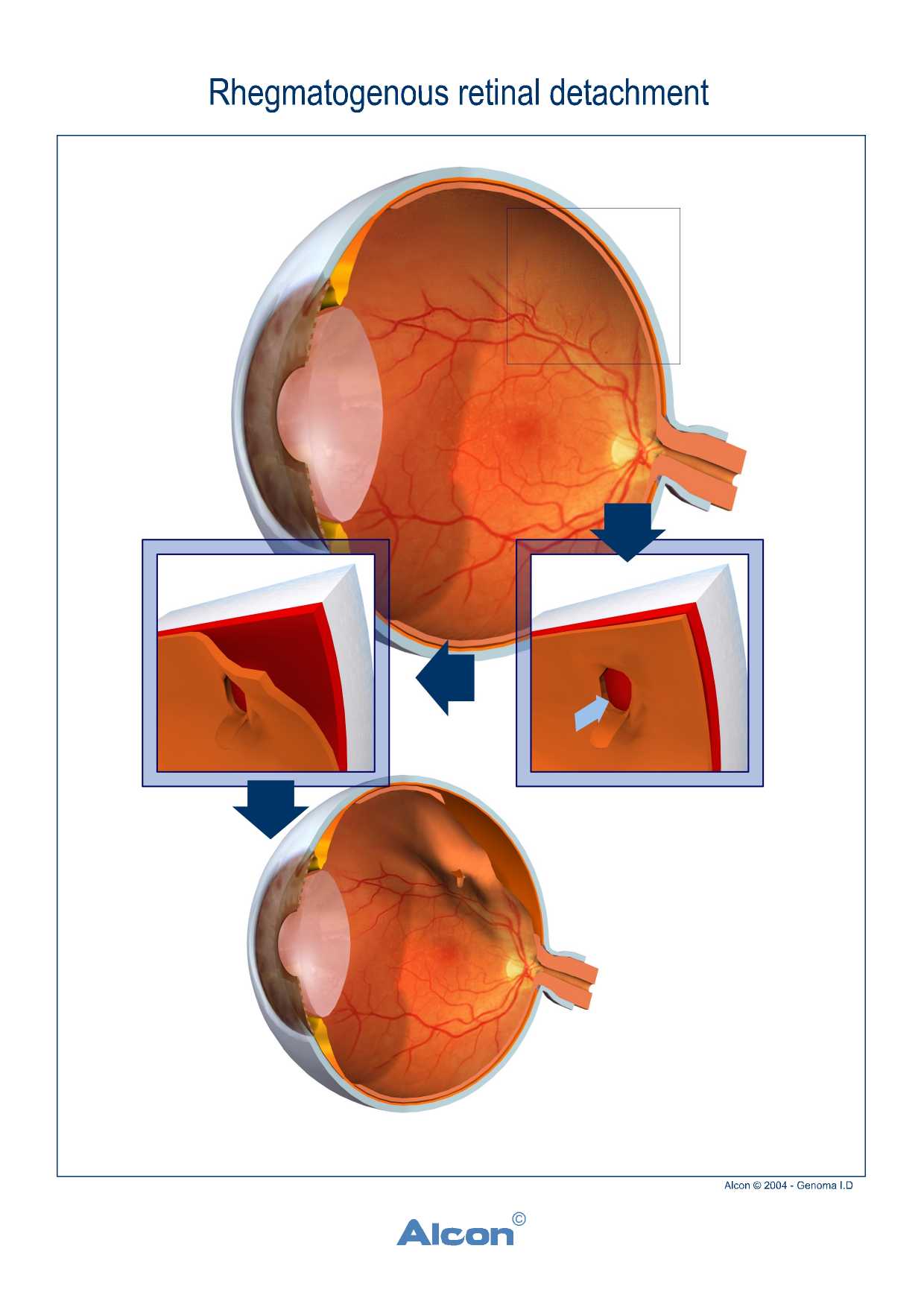
The most common type of retinal detachment is rhegmatogenous detachment. Mainly seen:
- After Injury
- In people with severe myopia - previously traumatized or not
- After cataract surgery
- In patients who had detachment in the other eye
- Or in patients with degenerative lesions of retinal periphery.
Patients describe either many "floaters" that suddenly appeared in front of the eyes, or a kind of "shadow or curtain", covering part of their field of vision.
What are the other types of retinal detachment?
More rare retinal detachment types can be:
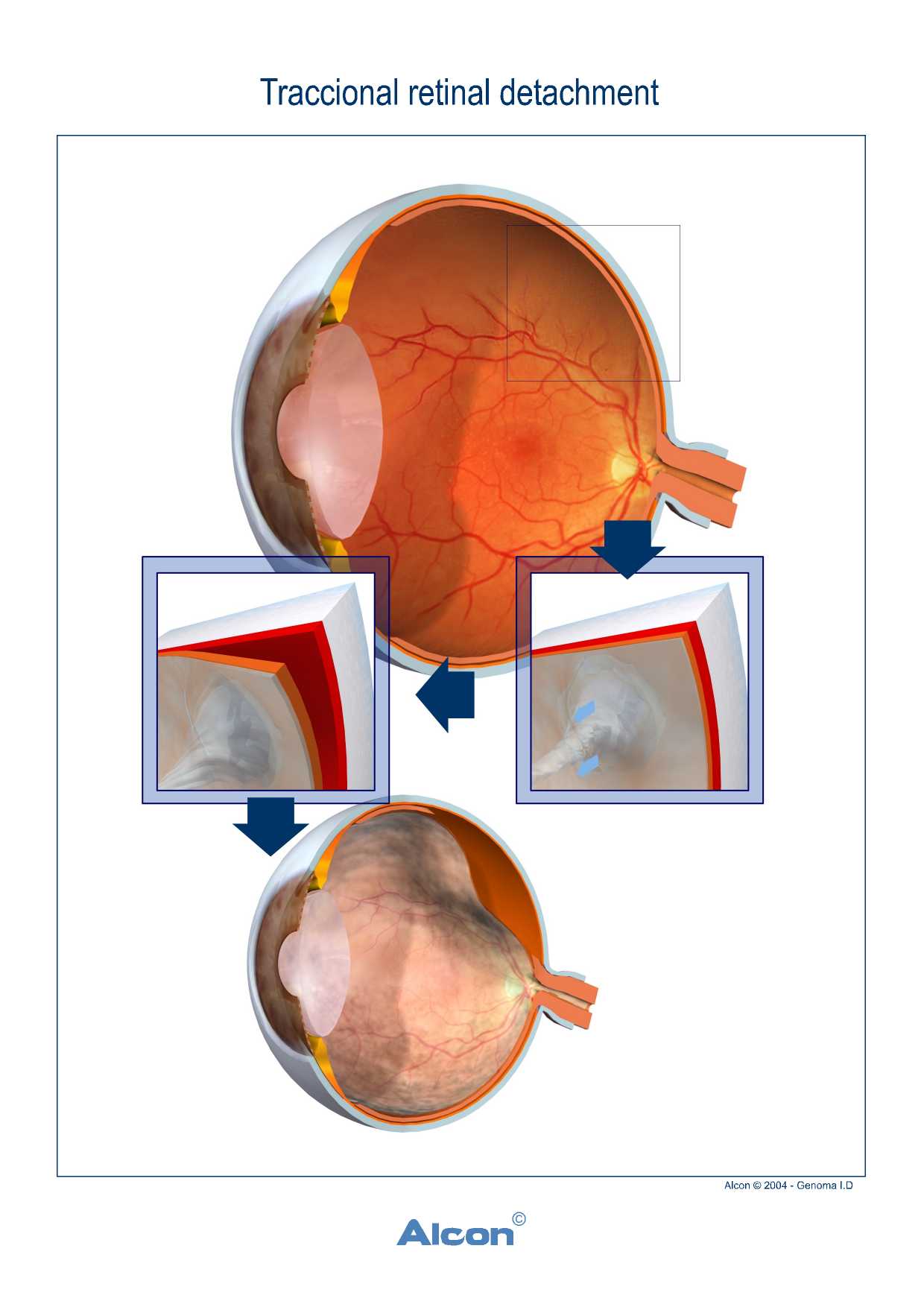
- Tractional
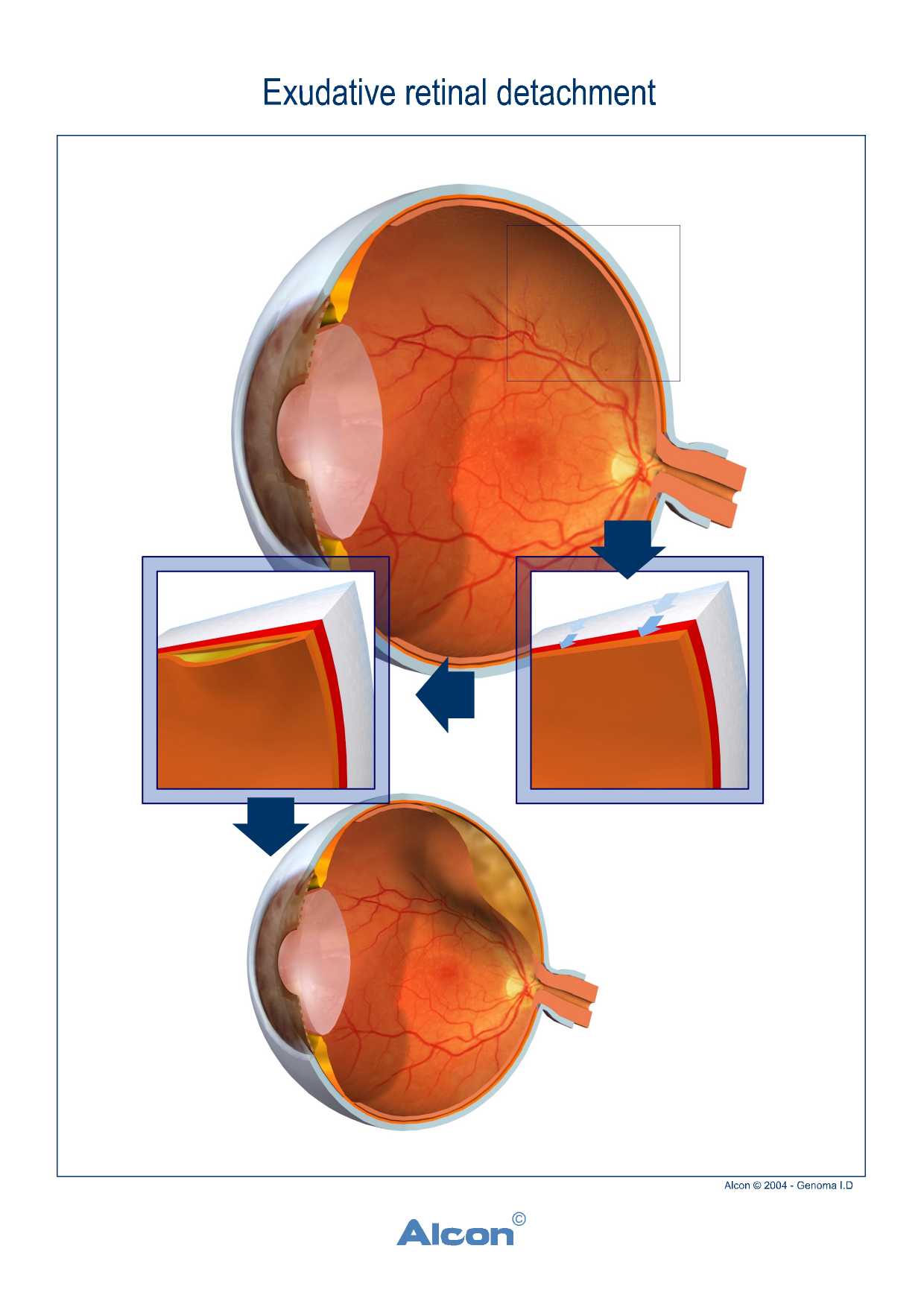
When fibrous tissue (for example in advanced diabetic retinopathy) contracts causing detachment due to traction (fig.3) or - Exudative
When the serous fluid (for example, in case of inflammation and retinal diseases), causes detachment, without the presence of a tear (fig.4).
 |
 |
Treatment
If the patient visits an ophthalmologist without delay and the retinal tear is repaired in time with laser treatment, the risk of retinal detachment is significantly reduced. However, if detachment occurs, surgery cannot be avoided. In the traditional and older method of retinal detachment treatment (which still has indications for use) the eye surgeon tries to press the sclera with a buckle inwards attaching again the 2 detached surfaces.
Alternatively the eye surgeons these days can remove the vitreous gel (vitrectomy) and replace it with special liquid or gas, in order to "flatten" the detached retina.
What should the patient do?
At the stage of a simple tear, patients do not need surgery and are treated only with laser treatment. However, in case of retinal detachment, surgery is the only option. In our country, we have experienced surgeons who specialize in the posterior segment of the eye and show excellent results. In conclusion, one should immediately visit an ophthalmologist if he/she develops 'floaters' or notice sudden reduction of vision. Early and accurate diagnosis increases the chances of an excellent outcome.
Digital content is courtesy of Prof.Oliver Findl www.findl.at
Digital content is courtesy of Alcon Iberia
Digital content: Credit to National Eye Institute, National Institutes of Health.




